Case Report 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Papilledema in Childhood for Diagnosis of Pseudotumor Cerebri or Late Hydrocephalus: A Case Report
*Corresponding author: Mariaelena Malvasi, Department of Sense Organs, Faculty of Medicine and Dentistry, Sapienza University of Rome, Italy.
Received: March 30, 2023; Published: April 10, 2023
DOI: 10.34297/AJBSR.2023.18.002476
Abstract
A case of hydrocephalus is presented in a 13-year-old female with transient loss of vision from 1 week and papilledema, previous ophthalmological history was negative. A visual field was performed, and neurological examination proved to be hydrocephalus. In literature few cases of Papilledema in adolescent children with hydrocephalus have been reported. The aim of this case report is to decode the signs, symptoms and factors associated with papilledema in children with hydrocephalus at an early stage in order to prevent a poor visual-functional residual (permanent low vision).
Introduction
Hydrocephalus most frequently results from Excessive Cerebrospinal Fluid (CSF) volume, with increased size of the cerebral ventricles and endocranial pressure, or from reduced brain mass due to degenerative diseases or congenital abnormalities. Etiopathogenesis is not yet fully known, probably resulting from an imbalance between production and absorption, most frequently with intraventricular accumulation of CSF. The case we describe is a form of tetra-ventricular late hydrocephalus, which, as reported in the literature, is rare and causes severe morbidity and death in children, which necessitates an early diagnosis, since although it presents a slow progression, the prognosis is generally inauspicious. It came to our attention in a 13-year-old girl, with general subjective symptoms: headache, stupor, disorientation, diplopia, and altered state of consciousness that had been present for a week, and ophthalmological disorders transient loss of Visual Acuity (AV) lasting a few seconds of recent onset to be attributed to the progressive papilledema. The diagnosis was made after performing all relevant clinical examinations, including comprehensive ophthalmic examination, neurological and neurosurgical evaluation, and instrumental examinations such as visual field (C.V.), bulbar ultrasound, Optical Coherence Tomography (OCT), brain RM. The purpose of this rare case report is to emphasize how early diagnosis and treatment are indispensable to avert the complications associated with the onset of papilledema with consequent irreversible loss of virus, as well as to describe the clinical presentation, which is of considerable neuro-ophthalmological and neurosurgical difficulty, and which represents a diagnostic challenge that requires teamwork to enable diagnosis to be made as soon as possible.
Case Report
A 13-year-old white woman, overweight (BMI=25), came to our observation, at the Fiorina Hospital in Terracina, Latina, Italy, Department of Ophthalmological Sciences, “La Sapienza” University of Rome, for ocular pain, photophobia, transient loss of AV in both eyes for 1 week, asthenia, drowsiness, and headache.
At the general anamnesis the patient reported, in particular, an increase in body weight and dysmenorrhea, the ophthalmological anamnesis no refractive defects were reported, nor previous ocular pathologies worthy of note, while for about 6 months divergent strabismus corrected with the use of prismatic lenses (prism 5 with internal base) and a VA of 10/10. The complete ophthalmological examination of our adolescents with papilledema included the valuation of Best Correct Visual Acuity (BCVA) which was 3/10 in right eye, and 4/10 in left eye, and which could not be improved with lenses. Color vision was generally compromised with the progression of the papilledema. The adnexa were intact, the anterior segment normal. Intraocular Pressure (IOP), measured with a Goldman applanation tonometer was 12 mmHg in both eyes. Fundus examination revealed the presence of marked papilledema with significant changes in its morphology. The oedema partially involved the posterior pole took on the typical star-shaped appearance with sparing of the macular region, the retina in the periphery was uninjured and on the plane.
The C.V. performed with Octopus 900 kinetic vectors perimeter, to assess and monitor any deficits and identify any imminent risk of visual function, showed concentric constriction of the isopters in both eyes, even if the execution of the examination is partially complete due to the symptoms in progress that did not allow a good collaboration of the patient.
It can be observed in the right eye, with the aim 1-4 exclusion of the blind spot, and in the left eye with the aim 1-3 an enlargement of the blind spot. At the OCT examination, performed with Heidelberg Spectral is system, there was no evidence of oedema in the macular area, while there was an increased thickness of the Retinal Nerve Fiber Layer (RNFL) with a value of 633 μm in right eye and 732μm in left eye. The clinical picture was compatible with Pseudotumor Cerebri (PTC). The bulb ultrasound in B-scan, performed with a 50 MHz probe showed virtual inhomogeneity. The increased value of the transverse diameter of the bilateral optic nerve head: right eye=5.97 mm and left eye =5.97 mm respectively from the retinal plane and marked accumulation of CSF in the subarachnoid periosteal spaces. To reduce the oedema of the posterior pole, the first treatment approach was conservative, with methylprednisolone sodium succinate 1g ev 1ml die for 3 days and Esomeprazole 20mg 1ml die. A new ophthalmological assessment was carried out on the second day of therapy, as the patient reported a worsening headache, accompanied by asthenia and chest pain, increased photophobia, persistent pain in both eyes, which confirmed the worsening of AV of 1/10 in the right eye and 2/10 in the left eye. The anterior segment was in the normal range and IOP of 12 mmHg in both eyes. The objectivity of the fundus examination revealed the persistence of oedema of the papilla with slight reduction (margins less blurred) the oedema involved the posterior pole and licked the macular region, while the retina in the periphery was unharmed. Performing a new C.V. showed increased constriction of the isopters in both eyes: the right eye presented a reduced visual field at 5° central with perimetric residual at 5° central, annular scotoma and the left eye presented a perimetric residual at 10° central, annular scotoma. On OCT the RNFL thickness was still above normal but decreased from the previous finding with a value (583μm in right eye, and 680μm in left eye).
A neurosurgical consultation and a brain RM with gadolinium was therefore immediately requested, which excluded the presence of cerebral neoplasms, stenosis and venous sinus thrombosis; showing instead increased ventricular spaces with accumulation of CSF in the optic sheaths to be referred to endocranial hypertension, empty Sella due to compression of the pituitary gland and herniation of the CSF-filled arachnoid diverticulum in the Sella turcica, the latter clinical sign was compatible with a pseudotumor cerebri form. Consequently, medical therapy with acetazolamide (Diamox) and Furosemide was carried out.
In view of the worsening visual acuity and clinical symptoms, and the lack of efficacy of medical therapy, after consultation and then the neurosurgical and ophthalmological diagnosis of Increased Intracranial Pressure (IPC), resulting from tetraventricular hydrocephalus; patients was candidate to surgery. In order to avert loss of vision, after informed consent of the parents, Helzinchi’s statement, the patient underwent ventricle-peritoneal shunt implantation surgery, through a right abdominal incision and tunnelling of the catheter at the right retro auricular level, a Prava 2 valve was connected. 0 (160 mmHg Shuntassisant 25 cmH20), then a right frontal pre-coronary flap was created. Then the catheter was introduced through a hole and the CSF leak was assessed, then the valve was connected, and function was checked at the abdominal level. Finally, the catheter was introduced into the peritoneum and attached to the superficial abdominal fascia.
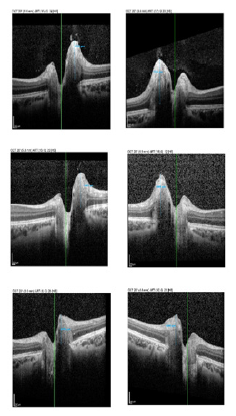
One week after surgery AV showed progressive improvement progressing by 2 Snellen lines in both eyes, with progressive improvement in the following months: after 1 month in both eyes BCVA 3/10, with suboptimal vision quality; IOP was 16 mmHG. The C.V father 1-month post-surgery showed improvement of the previously observed scotoma. Ophthalmoscopically the papilla showed gradual resolution of the oedema documented by OCT scans showing reduction in the thickness of the RNFL 476μm in right eye and 500μm in left eye. (Figure 1) shows the grey map of the visual field performed before and after surgery. (Figure 2) shows course of the RNFL thickness by measuring the same and (Figure 3) the respective optic disc Infrared (IR) images. Thickness trend of RNFL before and after surgery acquired by OCT execution is showed in (Figure 3) and the respective trend of optic disc Infrared (IR) images, before and after surgery, respective acquired during the OCT execution, which is representative of papilledema severity.
Discussion
Hydrocephalus is a condition caused by an imbalance between cerebrospinal fluid production and absorption; it can cause severe morbidity and death in children. Subjective symptoms in children in order of frequency are headache (57-87%), amaurosis fugax, blurred vision, pulsatile tinnitus, diplopia, transient visual loss of <30 sec (16-42.3%). Less frequently occurring are paresthesia’s, abducens paralysis (CN VI) 10-17%, back and lower limb pain 4-8%, nausea and vomiting 12.7-52%, arthralgias and unsteady gait, irritability, fatigue, and increased head circumference volume. [1] Sometimes these symptoms may be absent, particularly if ICP increases slowly, resulting in un specificity [2]. Papilledema is considered one of the most important signs of hydrocephalus and a determining factor in management strategy [3,4]. The absence of papilledema in younger infants with hydrocephalus can be attributed to the presence of open fontanelles, which in the newborn allow for the expansion of the skull and are protective against an increase in ICP, so that its increase is not sufficient to cause papilledema. [5,6]. In the literature, the incidence of papilledema has been estimated to be 14-50% in children with hydrocephalus caused by ventriculomegaly, and approximately 65% in children with hydrocephalus secondary to primary brain tumors. [3,7]. Papilledema is one of the most important signs of hydrocephalus and if undetected, can lead to irreversible damage up to blindness due to optic atrophy. The absence of papilledema may be a falsenegative sign [5]. Lee HJ et al. [8] reported absence of papilledema in 41% of children with hydrocephalus who were, however, younger than those with papilledema and it was also more common in older patients (mean age of 8.8±4.2 years) with higher ICP (of 33.3±9.1 cm H2O) with a mean symptom or sign of 3.4±3.9 months, the causes of which were recognised in order tumor (59%), congenital anomaly (19%), (19%), hemorrhage (13%) and infection (9%).

Figure 3:Trend of optic disc infrared (IR) images before and after surgery respective acquired during the OCT execution.
The duration of ICP elevation is an important factor in the development of papilledema [6]. In fact, pathophysiologically, the alteration that occurs in the optic nerve fibers during papilledema is the axonal swelling caused by the elevation of the ICP, with consequent impairment of axoplasmic flow. On the contrary in the case of acute elevation of ICP there is a blockage of both anterograde and retrograde axoplasmic flow that is not associated with swelling of the optic disc, for this reason papilledema is not considered a sensitive sign in the case of acute elevation of ICP. [6,9]. ICP associated with papilledema found in an overweight female adolescent, presented to our observation in the first instance with signs and symptoms typical of increased intracranial pressure, led us to hypothesize a case of Pseudotumor Cerebri (PTC) a condition in which the brain parenchyma is normal. In pediatric studies, the annual incidence of PTC is estimated at 0.6-0.71/100,000 [10-13]. Obesity is a risk factor that impacts beyond the age of 12 years, as it is closely related to pubertal status in the pathophysiology of primary PTC [14,15]. In contrast, in children under 12 years of age, weight does not seem to influence the development of PTC [16]. The diagnostic criteria for PTCS were revisited by Friedman et al. in 2013, our case did not present any features of a PTC [1] although it is reported in the literature that up to 53-78% of cases in children included obesity [11].
For the assessment and correlation of changes in optic nerve head volume and total retinal thickness with the degree of papilledema, instrumental examinations such as orbital ultrasonography and OCT [17] were performed in order to identify signs of optic neuropathy from ICP, and thus identify patients requiring timely treatment in order to preserve vision [18]. In fact, the following report describes the well-documented case of papilledema in an adolescent female patient with hydrocephalus and optic neuropathy from IPC, diagnosed through the appropriate instrumental support that showed dilatation of the ventricular spaces quickly, and excluded through a careful differential diagnosis with a PTC, whose clinical presentation in children varies with age and often takes on sometimes blurred pictures, which make diagnosis difficult.
The presence of papilledema in hydrocephalus is one of the most useful indicators for the preoperative diagnosis of increased intracranial pressure [11]. In fact, the extent of papilledema represented in our study an important criterion for the morphofunctional assessment of the therapeutic efficacy of medical therapy for ventriculo-peritoneal shunt surgery, as well as being considered as a criterion for post-operative follow-up. In accordance with the most recent literature, surgical treatment is currently the optimal therapeutic aid in hydrocephalus. In fact, the patient presented a marked improvement in visual acuity and objective picture following the ventriculoperitoneal shunt surgery. Indeed, it is essential to emphasise the importance of early diagnosis of hydrocephalus, even when it is present in these atypical forms, which may be suggested by the presence of papilledema. It is advisable for these patients to pay attention to visual symptoms and therefore to seek timely ophthalmic consultation, in order to preserve visual function, as chronic papilledema may lead to irreversible optic atrophy [19].
Acknowledgement
None.
Conflict of Interest
None.
References
- Friedman DI, Liu GT, Digre KB (2013) Revised diagnostic criteria for the pseudotumor cerebri syndrome in adults and children. Neurology 81(13): 1159-1165.
- Gaston H (1991) Ophthalmic complications of spina bifida and hydrocephalus. Eye (Lond) 5: 279-290.
- Corbett JJ (1986) Neuro-ophthalmologic complications of hydrocephalus and shunting procedures. Semin Neurol 6(2): 111-123.
- Newman NJ (1994) Bilateral visual loss and disc edema in a 15-year-old girl. Surv Ophthalmol 38: 365-370.
- Allen ED, Byrd SE, Darling CF, Tomita T, Wilczynski MA, et al. (1993) The clinical and radiological evaluation of primary brain tumors in children, Part I: Clinical evaluation. J Natl Med Assoc 85: 445-451.
- Nazir S, O Brien M, Qureshi NH, Slape L, Green TJ, et al. (2009) Sensitivity of papilledema as a sign of shunt failure in children. J AAPOS 13(1): 63-66.
- Mizrachi IB, Trobe JD, Gebarski SS, Garton HJ (2006) Papilledema in the assessment of ventriculomegaly. J Neuroophthalmol 26(4): 260-263.
- Lee HJ, Phi JH, Kim SK, Wang KC, Kim SJ, et al. (2017) Papilledema in children with hydrocephalus: incidence and associated factors. J Neurosurg Pediatr 19(6): 627-631.
- Steffen H, Eifert B, Aschoff A, Kolling GH, Völcker HE, et al. (1996) The diagnostic value of optic disc evaluation in acute elevated intracranial pressure. Ophthalmology 103(8): 1229-1232.
- Matthews YY, Dean F, Lim MJ, Mclachlan K, Rigby AS, et al. (2017) Pseudotumor cerebri syndrome in childhood: incidence, clinical profile and risk factors in a national prospective population-based cohort study. Arch Dis Child 102(8): 715-721.
- Barmherzig R, Szperka CL (2019) Pseudotumor Cerebri Syndrome in Children. Curr Pain Headache Rep 23(8): 58.
- Bursztyn LL, Sharan S, Walsh L, LaRoche GR, Robitaille J, et al (2014) Has rising pediatric obesity increased the incidence of idiopathic intracranial hypertension?. Can J Opthalmol 49(1): 87-91.
- Sheldon CA, Paley GL, Xiao R, Kesler A, Eyal O, et al. (2016) Pediatric Idiopathic Intracranial Hypertension: Age, Gender, and Anthropometric Features at Diagnosis in a Large, Retrospective, Multisite Cohort. Ophthalmology 123(11): 2424-2431.
- Rangwala LM, Liu GT (2007) Pediatric idiopathic intracranial hypertension. Surv Opthalmol 52(6): 597-617.
- Paley GL, Sheldon CA, Burrows EK, Chilutti MR, Liu GT, et al. (2015) Overweight and obesity in pediatric secondary pseudotumor cerebri syndrome. Am J Ophthalmol 159(2): 344-352.
- Standridge SM, O Brien SH (2008) Idiopathic intracranial hypertension in a pediatric population: a retrospective analysis of the initial imaging evaluation. J Child Neurol 23(11): 1308-1311.
- Gilbert AL, Heidary G (2016) Update on the evaluation of pediatric idiopathic intracranial hypertension. Curr Opin Ophthalmol 27(6): 493-497.
- Chen JJ, Thurntell MJ, Longmuir RA, Garvin MK, Wang JK, et al. (2015) Causes and prognosis of visual acuity loss at the time of initial presentation in idiopathic intracranial hypertension. Invest Opthalmol Vis Sci 56(6): 3850-3859.
- Selhorst JB, Gudeman SK, Butterworth JF IV, Harbison JW, Miller JD, et al. (1985) Papilledema after acute head injury. Neurosurgery 16(3): 357-363.




 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.